Abstract
Background
Antipsychotic medication is the mainstay of treatment in schizophrenia. Long-acting medication has potential advantages over daily medication in improving compliance and thus reducing hospitalization and relapse rates. The high acquisition and administration costs of such formulations raise the need for pharmacoeconomic evaluation.
Objective
The aim of this article is to provide a comprehensive review of the available evidence on the cost effectiveness of long-acting/extended-release antipsychotic medication and critically appraise the strength of evidence reported in the studies from a methodological viewpoint.
Methods
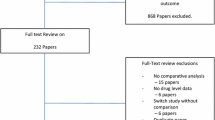
Relevant studies were identified by searching five electronic databases: PsycINFO, MEDLINE, EMBASE, the NHS Economic Evaluation Database and the Health Technology Assessment database (HTA). Search terms included, but were not limited to, ‘long-acting injection’, ‘economic evaluation’, ‘cost-effectiveness’ and ‘cost-utility’. No limits were applied for publication dates and language. Full economic evaluations on long-acting/extended-release antipsychotics were eligible for inclusion. Observational studies and clinical trials were also checked for cost-effectiveness information. Conference abstracts and poster presentations on the cost effectiveness of long-acting antipsychotics were excluded. Thirty-two percent of identified studies met the selection criteria. Pertinent abstracts were reviewed independently by two reviewers. Relevant studies underwent data extraction by one reviewer and were checked by a second, with any discrepancies being clarified during consensus meetings. Eligible studies were assessed for methodological quality using the quality checklist for economic studies recommended by the NICE guideline on interventions in the treatment and management of schizophrenia.
Results
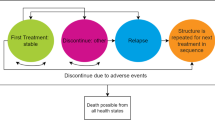
After applying the selection criteria, the final sample consisted of 28 studies. The majority of studies demonstrated that risperidone long-acting injection, relative to oral or other long-acting injectable drugs, was associated with cost savings and additional clinical benefits and was the dominant strategy in terms of cost effectiveness. However, olanzapine in either oral or long-acting injectable formulation dominated risperidone long-acting injection in a Slovenian and a US study. Furthermore, in two UK studies, the use of long-acting risperidone increased the hospitalization days and overall healthcare costs, relative to other atypical or typical long-acting antipsychotics. Finally, paliperidone extended-release was the most cost-effective treatment compared with atypical oral or typical long-acting formulations. From a methodological viewpoint, most studies employed decision analytic models, presented results using average cost-effectiveness ratios and conducted comprehensive sensitivity analyses to test the robustness of the results.
Limitations
Variations in study methodologies restrict consistent and direct comparisons across countries. The exclusion of a large body of potentially relevant conference abstracts as well as some papers being unobtainable may have increased the likelihood of misrepresenting the overall cost effectiveness of long-acting antipsychotics. Finally, the review process was restricted to qualitative assessment rather than a quantitative synthesis of results, which could provide more robust conclusions.
Conclusions
Atypical long-acting (especially risperidone)/extended-release antipsychotic medication is likely to be a cost-effective, first-line strategy for managing schizophrenia, compared with long-acting haloperidol and other oral or depot formulations, irrespective of country-specific differences. However, inconsistencies in study methodologies and in the reporting of study findings suggest caution needs to be applied in interpreting these findings.

Similar content being viewed by others
References
World Health Organization (WHO). The global burden of disease: 2004 update. 2008 [online]. http://www.who.int/healthinfo/global_burden_disease/estimates_regional/en/index.html. Accessed 15 May 2012.
Saha S, Chant D, Welham J, et al. A systematic review of the prevalence of schizophrenia. PLoS Med. 2005;2(5):e141.
McGrath J, Saha S, Welham J, et al. A systematic review of the incidence of schizophrenia: the distribution of rates and the influence of sex, urbanicity, migrant status and methodology. BMC Med. 2004;2:13.
Knapp M, Mangalore R, Simon J. The global costs of schizophrenia. Schizophr Bull. 2004;30(2):279–93.
American Psychiatric Association. Practice guideline for the treatment of patients with schizophrenia. Am J Psychiatry. 2004;161(Suppl. 2):1–56.
Jones PB, Barnes TR, Davies L, et al. Randomized controlled trial of the effect on quality of life of second- vs first-generation antipsychotic drugs in schizophrenia: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study (CUtLASS 1). Arch Gen Psychiatry. 2006;63(10):1079–87.
Leucht S, Wahlbeck K, Hamann J, et al. New generation antipsychotics versus low-potency conventional antipsychotics: a systematic review and meta-analysis. Lancet. 2003;361(9369):1581–9.
National Institute for Health and Clinical Excellence (NICE). National Clinical Guideline 82 on core interventions in the treatment and management of schizophrenia in adults in primary and secondary care [updated edition 2009]. http://publications.nice.org.uk/schizophrenia-cg82. Accessed 15 Apr 2012.
Lieberman JA, Stroup TS, McEvoy JP, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353(12):1209–23.
Almond S, Knapp M, Francois C, et al. Relapse in schizophrenia: costs, clinical outcomes and quality of life. Br J Psychiatry. 2004;184:346–51.
Joyce AT, Harrison DJ, Loebel AD, et al. Impact of atypical antipsychotics on outcomes of care in schizophrenia. Am J Manag Care. 2005;11(Suppl. 8):s254–61.
Heeg B, Buskens E, Botteman M, et al. The cost-effectiveness of atypicals in the UK. Value Health. 2008;11(7):1007–21.
Moore DB, Kelly DL, Sherr JD, et al. Rehospitalization rates for depot antipsychotics and pharmacoeconomic implications: comparison with risperidone. Am J Health Syst Pharm. 1998;55(Suppl. 4):s17–9.
Haycox A. Pharmacoeconomics of long-acting risperidone: results and validity of cost-effectiveness models. Pharmacoeconomics. 2005;23(Suppl. 1):3–16.
Keith S. Use of long-acting risperidone in psychiatric disorders: focus on efficacy, safety and cost-effectiveness. Expert Rev Neurother. 2009;9(1):9–31.
Fleischhacker WW, Eerdekens M, Karcher K, et al. Treatment of schizophrenia with long-acting injectable risperidone: a 12-month open-label trial of the first long-acting second-generation antipsychotic. J Clin Psychiatry. 2003;64(10):1250–7.
Chue PS, Heeg B, Buskens E, et al. Modelling the impact of compliance on the costs and effects of long-acting risperidone in Canada. Pharmacoeconomics. 2005;23(Suppl. 1):62–74.
Oh PI, Lanctot KL, Mittmann N, et al. Cost-utility of risperidone compared with standard conventional antipsychotics in chronic schizophrenia. J Med Econ. 2001;4:137–56.
Annemans L. Cost effectiveness of long-acting risperidone: what can pharmacoeconomic models teach us? Pharmacoeconomics. 2005;23(Suppl. 1):1–2.
Chue P. Long-acting risperidone injection: efficacy, safety, and cost-effectiveness of the first long-acting atypical antipsychotic. Neuropsychiatr Dis Treat. 2007;3(1):2007–39.
Fleischhacker WW. Second-generation antipsychotic long-acting injections: systematic review. Br J Psychiatry. 2009;52:s29–36.
Bartko G, Feher L. Pharmacoeconomic review of the use of injectable long-acting risperidone [Hungarian]. Neuropsychopharmacol Hung. 2005;7(4):199–207.
Bhanji NH, Chouinard G, Margolese HC. A review of compliance, depot intramuscular antipsychotics and the new long-acting injectable atypical antipsychotic risperidone in schizophrenia. Eur Neuropsychopharmacol. 2004;14(2):87–92.
Curran MP, Keating GM. Management of schizophrenia: defining the role of long-acting injectable risperidone. Dis Manag Health Outcomes. 2006;14(2):107–25.
Harrison TS, Goa KL. Spotlight on long-acting risperidone in schizophrenia. Am J Drug Deliv. 2004;2(3):L207–10.
Love RC, Conley RJ. Long-acting risperidone injection. Am J Health Syst Pharm. 2004;61:1792–800.
Purgato M, Adams CE. Bromperidol decanoate (depot) for schizophrenia. Cochrane Database Syst Rev. 2011;9(1):54.
De Graeve D, Smet A, Mehnert A, et al. Long-acting risperidone compared with oral olanzapine and haloperidol depot in schizophrenia: a Belgian cost-effectiveness analysis. Pharmacoeconomics. 2005;23(Suppl. 1):35–47.
Hensen M, Heeg B, Lthgren M, et al. Cost effectiveness of long-acting risperidone in Sweden. Appl Health Econ Health Policy. 2010;8(5):327–41.
Laux G, Heeg B, van Hout BA, et al. Costs and effects of long-acting risperidone compared with oral atypical and conventional depot formulations in Germany. Pharmacoeconomics. 2005;23:49–61.
Llorca PM, Miadi-Fargier H, Lancon C, et al. Cost-effectiveness analysis of schizophrenic patient care settings: impact of an atypical antipsychotic under long-acting injection formulation [French]. Encephale. 2005;31(2):235–46.
Yang YK, Tarn YH, Wang TY, et al. Pharmacoeconomic evaluation of schizophrenia in Taiwan: model comparison of long-acting risperidone versus olanzapine versus depot haloperidol based on estimated costs. Psychiatry Clin Neurosci. 2005;59(4):385–94.
Edwards NC, Rupnow MFT, Pashos CL, et al. Cost-effectiveness model of long-acting risperidone in schizophrenia in the US. Pharmacoeconomics. 2005;23(3):299–314.
Edwards NC, Locklear JC, Rupnow MF, et al. Cost effectiveness of long-acting risperidone injection versus alternative antipsychotic agents in patients with schizophrenia in the USA. Pharmacoeconomics. 2005;23(Suppl. 1):75–89.
Yang L, Li M, Tao LB, et al. Cost-effectiveness of long-acting risperidone injection versus alternative atypical antipsychotic agents in patients with schizophrenia in China. Value Health. 2009;12(Suppl. 3):66–9.
Heeg BM, Antunes J, Figueira ML, et al. Cost-effectiveness and budget impact of long-acting risperidone in Portugal: a modeling exercise. Curr Med Res Opin. 2008;24(2):349–58.
Mantovani LG, Berto P, D’ Ausilio A, et al. Costs and effects of Long Acting Risperidone (LAR) versus atypical antipsychotics in the treatment of schizophrenic subjects in Italy. Farmeconomia e percorsi terapeutici 2004;5(1):5–11.
Obradovic M, Mrhar A, Kos M. Cost-effectiveness of antipsychotics for outpatients with chronic schizophrenia. Int J Clin Pract. 2007;61(12):1979–88.
Baca E, Bobes J, Canas F, et al. Cost-effectiveness analysis of long-acting injectable risperidone v. olanzapine and v. fluphenazine decanoate in treating schizophrenia [Spanish]. Rev Esp Econ Salud 2005; 4(5):273–85.
Knapp M, Windmeijer F, Brown J, et al. Cost-utility analysis of treatment with olanzapine compared with other antipsychotic treatments in patients with schizophrenia in the pan-European SOHO study. Pharmacoeconomics. 2008;26(4):341–58.
Furiak NM, Ascher-Svanum H, Klein RW, et al. Cost-effectiveness of olanzapine long-acting injection in the treatment of patients with schizophrenia in the United States: a micro-simulation economic decision model. Curr Med Res Opin. 2011;27(4):713–30.
Edwards NC, Pesa J, Meletiche DM, et al. One-year clinical and economic consequences of oral atypical antipsychotics in the treatment of schizophrenia. Curr Med Res Opin. 2008;24(12):3341–55.
Garcia-Ruiz AJ, Perez-Costillias L, Montesinos AC, et al. Cost-effectiveness analysis of antipsychotics in reducing schizophrenia relapses. Health Econ Rev. 2012;2(1):8.
Geitona M, Kousoulakou H, Ollandezos M, et al. Costs and effects of paliperidone extended release compared with alternative oral antipsychotic agents in patients with schizophrenia in Greece: a cost effectiveness study. Ann Gen Psychiatry. 2008;7(16):1–12.
Barnett PG, Scott JY, Rosenheck RA. How do clinical trial participants compare to other patients with schizophrenia? Schizophr Res. 2011;130:34–9.
Niaz OS, Haddad PM. Thirty-five months experience of risperidone long-acting injection in a UK psychiatric service including a mirror-image analysis of in-patient care. Act Psychiatr Scand. 2007;116:36–46.
Carswell C, Wheeler A, Vanderpyl J, et al. Comparative effectiveness of long-acting risperidone: a report of resource utilisation and costs in a 12 month mirror-image analysis. Clin Drug Investig. 2010;30(11):777–87.
Chang HC, Tang CH, Huang ST, McCrone P, Su KP. A cost-consequence analysis of long-acting injectable risperidone in schizophrenia: a one-year mirror-image study with national claim-based database in Taiwan. J Psychiatr Res. 2012;46(6):751–6.
Spill B, Konoppa S, Kissling W, et al. Long-term observation of patients successfully switched to risperidone long-acting injectable: a retrospective, naturalistic 18-month mirror-image study of hospitalization rates and therapy costs. Int J Psychiatry Clin Pract. 2010;14(1):53–62.
Young CL, Taylor DM. Health resource utilization associated with switching to risperidone long-acting injection. Act Psychiatr Scand. 2006;114(1):14–20.
Olivares JM, Rodriguez-Martinez A, Buron JA, et al. Cost-effectiveness analysis of switching antipsychotic medication to long-acting injectable risperidone in patients with schizophrenia: a 12- and 24-month follow-up from the e-STAR database in Spain. Appl Health Econ Health Policy. 2008;6(1):41–53.
Taylor D, Fischetti C, Sparshatt A, et al. Risperidone long-acting injection: a 6-year mirror-image study of healthcare resource use. Act Psychiatr Scanda. 2009;120(2):97–101.
Knapp M. Costs of schizophrenia. Br J Psychiatry. 1997;171:509–18.
Leal A, Rosillon D, Mehnert A, et al. Healthcare resource utilization during 1-year treatment with long-acting, injectable risperidone. Pharmacoepidemiol Drug Saf. 2004;13(11):811–6.
Olivares JM, Peuskens J, Pecenak J, et al. Clinical and resource-use outcomes of risperidone long-acting injection in recent and long-term diagnosed schizophrenia patients: results from a multinational electronic registry. Curr Med Res Opin. 2009;25(9):2197–206.
McEvoy JP. Risks versus benefits of different types of long-acting injectable antipsychotics. J Clin Psychiatry. 2006;67(Suppl. 5):15–8.
Ginnelly L, Manca A. The use of decision models in mental health economic evaluation: challenges and opportunities. Appl Health Econ Health Policy. 2003;2(3):157–64.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. PLoS Med. 2009;6(7):1–28.
Acknowledgements
The authors would like to thank Leonardo Koeser and Hiong Tie (both researchers at the Centre for the Economics of Mental and Physical Health, King’s College, London) for their assistance in translating foreign-language papers.
Author contributions
Evanthia Achilla took the lead on conducting the review and writing the paper. Both Evanthia Achilla and Paul McCrone independently screened abstracts. Paul McCrone contributed to the writing of the paper and acts as guarantor of the content.
Conflicts of interest
This systematic review received no external funding. The authors declare no conflicts of interest. Paul McCrone has received honorarium from Janssen and Lilly for speaking at meetings.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Achilla, E., McCrone, P. The Cost Effectiveness of Long-Acting/Extended-Release Antipsychotics for the Treatment of Schizophrenia. Appl Health Econ Health Policy 11, 95–106 (2013). https://doi.org/10.1007/s40258-013-0016-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-013-0016-2