Abstract
Objective: To evaluate the efficacy and safety of guanfacine extended release (XR, Intuniv™; Shire Development Inc., Wayne, PA, USA) in the treatment of oppositional symptoms in children aged 6–12 years with a diagnosis of attention-deficit hyperactivity disorder (ADHD) and the presence of oppositional symptoms.
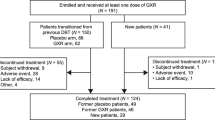
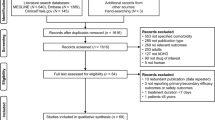
Subjects and Methods: In this randomized, double-blind, placebo-controlled, multicentre, flexible-dose, dose-optimization study, children aged 6–12 years were randomized to receive guanfacine XR (1–4mg/day) or placebo for 9 weeks. Screening and washout periods were followed by a 5-week dose-optimization period, a 3-week dose-maintenance period and a 1-week tapering period. The primary efficacy measure was change from baseline to endpoint in the oppositional subscale of the Conners’ Parent Rating Scale-Revised: Long Form (CPRS-R:L) score. Change in ADHD Rating Scale IV (ADHD-RS-IV) total score was a secondary efficacy measure. Safety assessments included adverse events (AEs), vital signs, ECG readings and laboratory studies.
Results: A total of 217 children were enrolled: 138 were randomized to receive guanfacine XR and 79 to receive placebo. Least-squares mean reductions from baseline to endpoint in CPRS-R:L oppositional subscale scores were 10.9 in the guanfacine XR group compared with 6.8 in the placebo group (p<0.001; effect size = 0.59). A significantly greater reduction in ADHD-RS-IV total score from baseline to endpoint was also seen in the guanfacine-treated group compared with the placebo group (23.8 vs 11.5, respectively; p<0.001; effect size = 0.92). A post hoc correlation analysis between percentage reduction from baseline to endpoint in CPRS-R:L oppositional subscale and ADHD-RS-IV total scores indicated that the decreases in oppositional symptoms and ADHD symptoms were highly correlated (r = 0.74).
The most commonly reported, treatment-emergent AEs (TEAEs) in the guanfacine XR group were somnolence (50.7%), headache (22.1%), sedation (13.2%), upper abdominal pain (11.8%) and fatigue (11.0%) and most were mild or moderate in severity. TEAEs of sedation, somnolence or hypersomnia were experienced by 62.5% of subjects in the guanfacine XR group. These events were most common during the dose-titration period but most (63.5%) resolved prior to the taper period. TEAEs of fatigue, lethargy and asthenia were reported in 11.0%, 3.7% and 0.0% of subjects in the guanfacine XR group, respectively. Most subjects receiving guanfacine XR demonstrated modest changes in blood pressure, pulse rate and ECG readings that were not considered clinically significant.
Conclusions: In this population of children aged 6–12 years with ADHD and the presence of oppositional symptoms, significant reductions in CPRS-R:L oppositional subscale and ADHD-RS-IV total scores were observed with guanfacine XR treatment compared with placebo. Treatment with guanfacine XR at optimized doses was associated with mostly mild or moderate TEAEs. The findings of this study support the efficacy of guanfacine XR in the treatment of children with ADHD and the presence of oppositional symptoms.
Clinical Trial Registration Number: NCT00367835.







Similar content being viewed by others
References
American Psychiatric Association. Disorders usually first diagnosed in infancy, childhood and adolescence. In: Diagnostic and statistical manual of mental disorders. 4th ed. Text revision. Washington, DC: American Psychiatric Association, 2000: 85–93
Reiff MI, Stein MT. Attention-deficit/hyperactivity disorder evaluation and diagnosis: a practical approach in office practice. Pediatr Clin North Am 2003 Oct; 50(5): 1019–48
Biederman J, Faraone SV. Attention-deficit hyperactivity disorder. Lancet 2005 Jul; 366(9481): 237–48
Centers for Disease Control and Prevention. Mental health in the United States: prevalence of diagnosis and medication treatment for attention-deficit/hyperactivity disorder: United States, 2003. MMWR Morb Mortal Wkly Rep 2005 Sep; 54(34): 842–7
Biederman J, Faraone SV, Milberger S, et al. Is childhood oppositional defiant disorder a precursor to adolescent conduct disorder? Findings from a four-year follow-up study of children with ADHD. J Am Acad Child Adolesc Psychiatry 1996 Sep; 35(9): 1193–204
Pliszka SR, Carlson CL, Swanson JM. Disruptive behavior disorders and substance abuse. In: Pliszka SR, Carlson CL, Swanson JM. ADHD with comorbid disorders: clinical assessment and management. New York: The Guilford Press, 1999: 89-112
Biederman J. Attention-deficit/hyperactivity disorder: a selective overview. Biol Psychiatry 2005 Jun; 57(11): 1215–20
Steiner H, Remsing L, AACAP Work Group on Quality Issues. Practice parameter for the assessment and treatment of children and adolescents with oppositional defiant disorder. J Am Acad Child Adolesc Psychiatry 2007 Jan; 46(1): 126–41
Connor DF, Doerfler LA. ADHD with comorbid oppositional defiant disorder or conduct disorder; discrete or nondistinct disruptive behavior disorders? J Atten Disord 2008; 12: 126–34
Barkley RA, Guevremont DC, Anastopoulos AD, et al. Driving-related risks and outcomes of attention deficit hyperactivity disorder in adolescents and young adults: a 3- to 5-year follow-up survey. Pediatrics 1993 Aug; 92(2): 212–8
Harpold T, Biederman J, Gignac M, et al. Is oppositional defiant disorder a meaningful diagnosis in adults? Results from a large sample of adults with ADHD. J Nerv Ment Dis 2007 Jul; 195(7): 601–5
Klassen AF, Miller A, Fine S. Health-related quality of life in children and adolescents who have a diagnosis of attention-deficit/hyperactivity disorder. Pediatrics 2004 Nov; 114(5): e541–7
Connor DF, Glatt SJ, Lopez ID, et al. Psychopharmacology and aggression: I. A meta-analysis of stimulant effects on overt/covert aggression-related behaviors in ADHD. J Am Acad Child Adolesc Psychiatry 2002 Mar; 41(3): 253–61
Spencer TJ, Abikoff HB, Connor DF, et al. Efficacy and safety of mixed amphetamine salts extended release (Adderall XR) in the management of oppositional defiant disorder with or without comorbid attention-deficit/ hyperactivity disorder in school-aged children and adolescents: a 4-week, multicenter, randomized, double-blind, parallel-group, placebo-controlled, forced-dose-escalation study. Clin Ther 2006 Mar; 28(3): 402–18
Connor DF. Pharmacological treatment of ODD symptoms in ADHD children: a brief review. ADHD Report 2007; 15(1): 1–6
Goez H, Back-Bennet O, Zelnik N. Differential stimulant response on attention in children with comorbid anxiety and oppositional defiant disorder. J Child Neurol 2007 May; 22(5): 538–42
Newcorn JH, Spencer TJ, Biederman J, et al. Atomoxetine treatment in children and adolescents with attention-deficit/hyperactivity disorder and comorbid oppositional defiant disorder. J Am Acad Child Adolesc Psychiatry 2005 Mar; 44(3): 240–8
Hoffenaar PJ, Hoeksma JB. The structure of oppositionality: response dispositions and situational aspects. J Child Psychol Psychiatry 2002 Mar; 43(3): 375–85
Philipsen A. Differential diagnosis and comorbidity of attention-deficit/hyperactivity disorder (ADHD) and borderline personality disorder (BPD) in adults. Eur Arch Psychiatry Clin Neurosci 2006 Sep; 256 Suppl. 1: i42–6
Barkley RA. Behavioral inhibition, sustained attention, and executive functions: constructing a unifying theory of ADHD. Psychol Bull 1997 Jan; 121(1): 65–94
Roth RM, Saykin AJ. Executive dysfunction in attention-deficit/hyperactivity disorder: cognitive and neuroimaging findings. Psychiatr Clin North Am 2004 Mar; 27(1): 83–96
Willcutt EG, Doyle AE, Nigg JT, et al. Validity of the executive function theory of attention-deficit/hyperactivity disorder: a meta-analytic review. Biol Psychiatry 2005 Jun; 57(11): 1336–46
Arnsten AF, Scahill L, Findling RL. Alpha-2 adrenergic receptor agonists for the treatment of attention-deficit/ hyperactivity disorder: emerging concepts from new data. J Child Adolesc Psychopharmacol 2007; 17(4): 393–406
Intuniv™ (guanfacine extended-release tablets): US prescribing information. Wayne (PA): Shire Pharmaceuticals Inc., 2009
Biederman J, Melmed RD, Patel A, et al., for the SPD503 Study Group. A randomized, double-blind, placebo-controlled study of guanfacine extended release in children and adolescents with attention-deficit/hyperactivity disorder. Pediatrics 2008; 121(1): e73–84
Sallee F, McGough J, Wigal T, et al., for the SPD503 Study Group. Guanfacine extended release in children and adolescents with attention-deficit/hyperactivity disorder: a placebo-controlled trial. J Am Acad Child Adolesc Psychiatry 2009; 48(2): 155–65
Arnsten AFT, Li B-M. Neurobiology of executive functions: catecholamine influences on prefrontal cortical functions. Biol Psychiatry 2005 Jun; 57(11): 1377–84
Arnsten AF, Dudley AG. Methylphenidate improves prefrontal cortical cognitive function through α2 adrenoceptor and dopamine D1 receptor actions: relevance to therapeutic effects in attention deficit hyperactivity disorder [letter]. Behav Brain Funct 2005 Apr; 1(1): 2
Arnsten AFT. Stimulants: therapeutic actions in ADHD. Neuropsychopharmacology 2006 Nov; 31(11): 2376–83
Berridge CW, Stalnaker TA. Relationship between low-dose amphetamine-induced arousal and extracellular norepinephrine and dopamine levels within prefrontal cortex. Synapse 2002 Dec; 46(3): 140–9
Berridge CW, Devilbiss DM, Andrzejewski ME, et al. Methylphenidate preferentially increases catecholamine neurotransmission within the prefrontal cortex at low doses that enhance cognitive function. Biol Psychiatry 2006 Nov; 60(10): 1111–20
Franowicz JS, Kessler LE, Borja CM, et al. Mutation of the α2A-adrenoceptor impairs working memory performance and annuls cognitive enhancement by guanfacine. J Neurosci 2002 Oct; 22(19): 8771–7
Uhlén S, Wikberg JES. Delineation of rat kidney α2A- and α2B-adrenoceptors with [3H]RX821002 radioligand binding: computer modelling reveals that guanfacine is an α2A-selective compound. Eur J Pharmacol 1991 Sep; 202(2): 235–43
Arnsten AFT, Cai JX, Goldman-Rakic PS. The alpha-2 adrenergic agonist guanfacine improves memory in aged monkeys without sedative or hypotensive side effects: evidence for alpha-2 receptor subtypes. J Neurosci 1988 Nov; 8(11): 4287–98
Newcorn JH, Schulz K, Harrison M, et al. α2-Adrenergic agonists: neurochemistry, efficacy, and clinical guidelines for use in children. Pediatr Clin North Am 1998 Oct; 45(5): 1099–122
Conners CK. Conners’ Rating Scales-Revised technical manual. North Tonawanda (NY): Multi-Health Systems Inc., 2001
Mozzicato P. MedDRA: an overview of the medical dictionary for regulatory activities. Int J Pharm Med 2009 Apr 1; 23(2): 65–75
US Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research, et al. Guidance for industry: E14 clinical evaluation of QT/QTc interval prolongation and proarrhythmic potential for non-antiarrhythmic drugs. ICH E14 [online]. Available from URL: http://www.fda.gov/downloads/RegulatoryInformation/Guidances/UCM129351.pdf [Accessed 2010 Jan 14]
Bangs ME, Hazell P, Danckaerts M, et al. Atomoxetine for the treatment of attention-deficit/hyperactivity disorder and oppositional defiant disorder. Pediatrics 2008 Feb; 121(2): e314–20
Kolko DJ, Bukstein OG, Barron J. Methylphenidate and behavior modification in children with ADHD and comorbid ODD or CD: main and incremental effects across settings. J Am Acad Child Adolesc Psychiatry 1999 May; 38(5): 578–86
Connor DF, Barkley RA, Davis HT. A pilot study of methylphenidate, clonidine, or the combination in ADHD comorbid with aggressive oppositional defiant or conduct disorder. Clin Pediatr 2000 Jan; 39(1): 15–25
Gadow KD, Nolan EE, Sverd J, et al. Methylphenidate in children with oppositional defiant disorder and both comorbid chronic multiple tic disorder and ADHD. J Child Neurol 2008 May; 23: 981–90
Serra-Pinheiro MA, Mattos P, Souza I, et al. The effect of methylphenidate on oppositional defiant disorder comorbid with attention deficit/hyperactivity disorder. Arq Neuropsiquiatr 2004 Jun; 62(2B): 399–402
Steere JC, Arnsten AF. The alpha-2A noradrenergic receptor agonist guanfacine improves visual object discrimination reversal performance in aged rhesus monkeys. Behav Neurosci 1997 Oct; 111(5): 883–91
Kollins SH, Wigal T, Vince B, et al. Cognitive and sedative effects of guanfacine extended release in children and adolescents aged 6 to 17 years with attention-deficit/ hyperactivity disorder. Poster presented at Society of Biological Psychiatry 63rd Annual Scientific Meeting; 2008 May 1–3, Washington, DC
Gorman EB, Klorman R, Thatcher JE, et al. Effects of methylphenidate on subtypes of attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 2006 Jul; 45(7): 808–16
Palumbo DR, Sallee FR, Pelham Jr WE, et al., and the CAT Study Team. Clonidine for attention-deficit/hyperactivity disorder: I. Efficacy and tolerability outcomes. J Am Acad Child Adolesc Psychiatry 2008 Jan; 47(2): 180–8
Kelsey DK, Sumner CR, Casat CD, et al. Once-daily atomoxetine treatment for children with attention-deficit/ hyperactivity disorder, including an assessment of evening and morning behavior: a double-blind, placebo-controlled trial. Pediatrics 2004 Jul; 114(1): e1–8
Michelson D, Allen AJ, Busner J, et al. Once-daily atomoxetine treatment for children and adolescents with attention deficit hyperactivity disorder: a randomized, placebo-controlled study. Am J Psychiatry 2002 Nov; 159(11): 1896–901
Spencer T, Heiligenstein JH, Biederman J, et al. Results from 2 proof-of-concept, placebo-controlled studies of atomoxetine in children with attention-deficit/hyperactivity disorder. J Clin Psychiatry 2002 Dec; 63(12): 1140–7
Faraone SV. Understanding the effect size of ADHD medications: implications for clinical care [online]. Available from URL: http://www.medscape.com/viewarticle/461543 [Accessed 2008 Sep 23]
Greenhill LL, Biederman J, Boellner SW, et al. A randomized, double-blind, placebo-controlled study of modafinil film-coated tablets in children and adolescents with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 2006 May; 45(5): 503–11
Conners CK, Casat CD, Gualtieri CT, et al. Bupropion hydrochloride in attention deficit disorder with hyper-activity. J Am Acad Child Adolesc Psychiatry 1996 Oct; 35(10): 1314–21
Connor DF, Fletcher KE, Swanson JM. A meta-analysis of clonidine for symptoms of attention-deficit hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 1999 Dec; 38(12): 1551–9
Biederman J, Spencer TJ, Newcorn JH, et al. Effect of comorbid symptoms of oppositional defiant disorder on responses to atomoxetine in children with ADHD: a meta-analysis of controlled clinical trial data. Psychopharmacology (Berl) 2007 Jan; 190(1): 31–41
Acknowledgements
This clinical research was funded by Shire Development Inc. Authors directed writing assistance from Jennifer Steeber, PhD, an employee of Health Learning Systems. Editorial assistance in the form of proofreading, copy editing and fact checking was also provided by Health Learning Systems. Health Learning Systems was funded by Shire Development Inc. for authorship support in writing and editing this manuscript. Although the sponsor was involved in the design, collection, analysis, interpretation and fact checking of information, the ultimate interpretation was made by the independent authors, as was the content of this manuscript and the decision to submit it for publication in CNS Drugs.
Dr Daniel F. Connor receives honoraria and grant research support from Shire Pharmaceuticals, Inc. and is a speaker, consultant and is on the advisory board for Shire Pharmaceuticals, Inc. He also receives support from NIMH and the State of Connecticut, USA.
Dr Robert L. Findling receives or has received research support, acted as a consultant and/or served on a speaker’s bureau for Abbott, Addrenex, AstraZeneca, Biovail, Bristol-Myers Squibb, Forest, GlaxoSmithKline, Johnson & Johnson, KemPharm Lilly, Lundbeck, Neuropharm, Novartis, Organon, Otsuka, Pfizer, sanofi-aventis, Sepracor, Shire Pharmaceuticals, Inc., Solvay, Supernus Pharmaceuticals, Validus and Wyeth.
Dr Scott H. Kollins has received research support and/or consultant fees from Shire Laboratories Inc., Addrenex Pharmaceuticals Inc., CoMentis Inc., the National Institute on Drug Abuse, the National Institute of Mental Health, the National Institute of Environmental Health Sciences, the National Institute of Neurological Disorders and Strokes, and the Environmental Protection Agency.
Dr Floyd Sallee receives funding through consultancies from AstraZeneca, Otsuka, P2D Inc., Sepracor and Shire Pharmaceuticals, Inc. and honoraria from Shire Pharmaceuticals, Inc. He has stock ownership and is a member of the board of directors for P2D Inc. Dr Sallee has given expert testimony on behalf of Johnson & Johnson and Sun Pharma. He has a patent pending on behalf of the University of Cincinnati and is a founder of Satiety Solutions, LLC.
Dr Frank A. López is a consultant for Celltech, Cephalon, Eli Lilly, New River, Novartis and Shire Pharmaceuticals, Inc. He has received honoraria from Novartis and Shire Pharmaceuticals, Inc. He has received grants from Bristol-Myers Squibb, Celltech, Cephalon, New River, Novartis, Pfizer and Shire Pharmaceuticals Inc.
Andrew Lyne is a full-time employee of Shire Pharmaceutical Development Ltd, Basingstoke, UK.
Dr Gerald Tremblay is a full-time employee of Shire Development Inc., Wayne, PA, USA.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Connor, D.F., Findling, R.L., Kollins, S.H. et al. Effects of Guanfacine Extended Release on Oppositional Symptoms in Children Aged 6–12 Years with Attention-Deficit Hyperactivity Disorder and Oppositional Symptoms. CNS Drugs 24, 755–768 (2010). https://doi.org/10.2165/11537790-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11537790-000000000-00000